COMPLEX IMPLANT SITE & FRESH EXTRACTION SOCKET– Challenge or Essence? For A High Torque Bi-directional Bone Cutting BLX Implant
Feb 3
/
Dr. Tak-Kun CHOW
The purpose of this report is to present a 30 months experience in using a high torque bi-directional bone cutting implant in a private oral & maxillofacial surgery practice since March 2020. Promising clinical outcome in complex sites including fresh extraction socket for immediate implant placement by this newly evolved implant was evidenced by follow up x-ray and Cone Beam CT monitoring. In this cohort of patients, thorough analyze the pattern of the complex sites & immediate implant to fresh extraction sockets to elucidate the sophistication of the implant design & its biomechanical innovations.
The outcome of conventional staged protocol for dental implant osseointegration has been shown to be highly predictable and successful regardless many different designs and brands of implants1 - 3.
Result
DISCUSSION
Traditional guidelines suggested 2 to 3 months of socket remodeling following tooth extraction and further 3 to 6 months of load-free healing after implant insertion were needed for optimal osseointegration13. Such a long rehabilitation time jeopardize the patient’s quality of life especially in the aesthetic demand region. The social and economic impact of reduction in number of surgical procedures and in treatment time is unequivocal.
Not until recently, more long-term scientific evidences5 were presented to acknowledge the immediate post-extraction implant placement which is a predictable implant alternative with a survival rate similar to that of the conventional technique for implant placement. And yet it still categorized as a high risk of implant failure in comparison to delayed implants14.
Inevitability, earliest implant rehabilitation could relieve both psychosocial and oral dental functional impact to patient after tooth lost, and that should be the parameter of care in contemporary implant dentistry.
Immediate implant placement in fresh extraction socket is a technique that has been developed, especially within the last decade, although it could be dated back to late 1970s at the University of Tubingen, an implant model was specially designed for such procedure4. In recent years, there has been an increase in the number of studies on immediate placement which present their results a high success rate of osseointegration as comparable to conventional staged approach5. To secure a predictable outcome, the clinician should well master the bio-physiology of fresh extraction socket healing in addition to the initial stability of implant placement. Primary or initial Implant stability is of paramount important for implant placement in fresh extraction sockets and immediately loaded6. Variable-thread implant with its feature of high insertion torque7 enhancing immediate implant placement was introduced. Surface technologies8,9 to enhance immediate placement such as the TiUnite rough-surfaced, nanostructures found on Ti-Zr hydrophilic SLActive® surfaces had been well described to promote osseointegration. Until 2019, a new generation BLX self-drilling implants10 has been introduced by Fromovich O et al that could have dynamic bone management and a combination of Roxolid alloy® and SLActive® surface specially for immediate placement and loading purpose so as application in complex recipient sites. Complex sites commonly encounter in our daily practice that is either a severely resorbed extraction socket or disease involved socket that could be devastating if not properly grafted or prepared. Kim et al has devised a new classification11 on 5 types of compromised extraction sockets according to destruction of hard and soft tissue. Similar kind of classification by Chang & Cheng12 could help the implant dentist to follow a treatment algorithm. Furthermore, other complex situation such as localized ridge deformities or patient with systemic disease such as chemotherapy or radiotherapy would also complicate the treatment outcome.
The purpose of this report is to present a 30 months’ consecutive series in using a high torque bi-directional thread implant in a private oral & maxillofacial surgery practice since March 2020. Promising outcome in complex extraction sites including fresh extraction socket for immediate implant placement by this newly evolved implant was evidenced by follow up x-ray and Cone Beam CT monitoring. In this case series, thorough analyze the pattern of the complex extraction sites to illustrate the sophistication of implant design to achieve such a promising result.
Materials & Methods
Materials & Methods
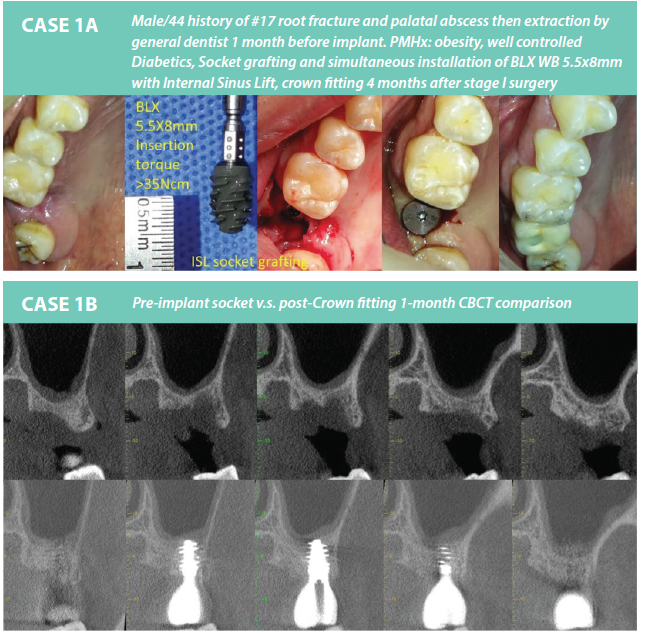
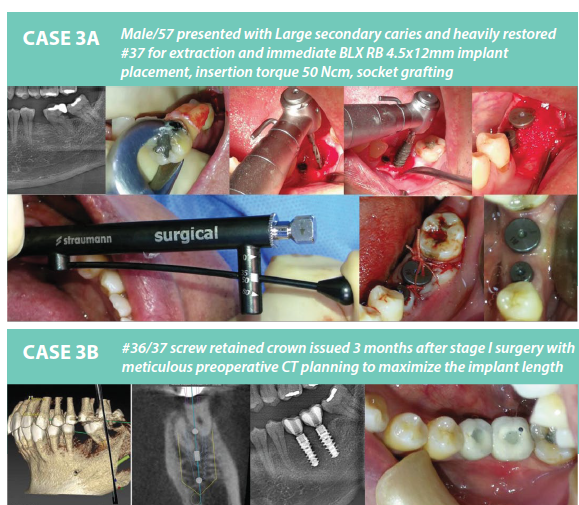
45 implants were placed in 21 patients for comprehensive prosthodontics rehabilitation in a private oral maxillofacial surgery specialist practice according to a standard protocol since March 2020 till September 2022. 19 implants were placed immediately after extraction whilst 8 of them were immediate functionally loaded with provisional restoration. (Table 1) Nevertheless 19 implants were installed to namely ‘Complex sites’ need localized bone grafting due to either anatomical, severe bone lost due to dental pathosis or patient with systemic disease background. (Table 2) Clinical and radiographic assessment was performed regularly after implant placement at 6 months, 12 months, and 24 months interval.
Table 1. Immediate Extraction & Implant placement into Fresh Extraction Socket
Table 1. Immediate Extraction & Implant placement into Fresh Extraction Socket
| Region | Tooth Position | Implant size (mm) |
| Incisor Region -6 BLX | 21/12/22/31/42/11 | 3.75x12/3.75x14/3.75x14/ 3.75x12/3.75x12/4x14 |
| Premolar Region -8 BLX | 35/44/45/45/25/35/45/35 | 4.5x12/4.0x12/4.0x12/5.0x8/ 4.0x12/4.5x8/4.5x8/4.5x12 |
| Molar Region -5 BLX | 46/46/37/46/46 | 5.5x12/5.0x12*/4.5x12/4.5x12/4.5x12 |
Result
21patients were treated with 45 Straumann® BLX implants and were restored with either single crowns or multi-unit bridges. The male-to-female ratio was 12:9, with a mean age of 55.4 years ± 11.6 (range 23-73). The mean follow-up time post-surgery was 10.74 months ± 8.09 (range 1-28) as of September 2022. The follow-up included observing clinically immobile implants, negative radiographic peri-implant bone loss, no persistent pain or infection, and a stable gingival complex.
Among the implants, 19 (42%) were placed immediately after extraction, and 8 of these were immediately functional with provisional restoration. Nineteen implant fixtures (42%) were installed in "complex sites." Immediate implant placement in fresh extraction sockets was predominantly in premolars (42.1%, 8 implants), followed by incisors (31.5%, 6 implants) and molars (26.3%, 5 implants). Thus, 84.2% (16 implants) of immediate implants were longer than 12mm to secure primary stability with insertion torque > 35Ncm. Peri-implant gaps to the extraction socket wall >1.5mm were grafted with purified cancellous bovine bone mineral granules with porcine collagen (Creos™) and further secured by peri-gingival suturing.
Table 2 shows the pattern of the "complex sites," where 6 sites already had Creos™ socket grafting or ridge augmentation for at least 3 months before stage I implant surgery but still needed adjunct procedures such as localized bone grafting or internal sinus lift. Three fixtures were installed at former benign bone tumor excision areas and bone-grafted cleft alveolus for dental rehabilitation purposes. Furthermore, two patients with a history of cancer had chemotherapy or radiation therapy, receiving a total of 6 dental implants. Unfortunately, one implant failed in a patient with a background of chemotherapy and chronic smoking at a grafted premolar socket.
The overall survival rate was encouraging at 97.8% (44/45). All immediate implants into fresh extraction sockets, with or without immediate functional loading, were 100% successful. Until mid-September 2022, one molar immediate implant crown experienced prosthetic failure due to abutment fracture after 18 months of functional loading, resulting in an overall success rate of 95.6% (43/45).
Table 2.Complex Sites Profile Analysis: 19 sites in 13 patients
Table 2.Complex Sites Profile Analysis: 19 sites in 13 patients
| Patient | Complexity | No | Implant size | Implant placement | Adjunct grafting | Outcome |
| 1 | Medical - Cancer chemotherapy history | 2 | (#15)*3.75x6mm,(#14)4x5mm | Post socket grafting implant placement | Yes | (#15)#infected Failure (#14) success |
| 2 | Medical - NPC Cancer history with RT | 4 | (#11)4x14mm+ (#25)4x12mmimmediate ex & implant> (#46)4.5x10mm+(#35)4x10mm< Standard 2-stage implant placement> | Immed ex &place (#11.25) Standard 2-stage (#46,35) | No | Success |
| 3 | Medical - Benign tumor excision site | 2 | (#14)4.5x12mm (#15)5.5x8mm | Standard 2-stage implant placement | No | Success |
| 4 | Medical - Cleft alveolus site | 1 | (#21)4x12mm | Standard 2-stage implant placement | Yes | Success |
| 5-8 | Advanced periodontal bone lost just above mental foramen or maxilla sinus | 4 | (#45)5x8mm (#35)4.5x8,(#45)4.5x8 (#17)'5.5x8mm need Internal Sinus lift ISL of a delay ex socket> | Immed ex & placement | Yes | Success |
| 9-12 | Severely resorbed extraction socket grafting >3m (periapical infection) | 4 | (#17)5x6mm (#15)4.5x6mm (#16)5.5x6mm (#25)5x6mm | Standard 2-stage implant placement | No | Success |
| 13 | Atrophic alveolus after unsuccessful sinus grafting | 2 | (#15)5x8mm+(#16)4.5x8mm <need Intemal Sinus lift ISL> | Standard 2-stage implant placement | Yes+ISL | Success |
DISCUSSION
Traditional guidelines suggested 2 to 3 months of socket remodeling following tooth extraction and further 3 to 6 months of load-free healing after implant insertion were needed for optimal osseointegration13. Such a long rehabilitation time jeopardize the patient’s quality of life especially in the aesthetic demand region. The social and economic impact of reduction in number of surgical procedures and in treatment time is unequivocal.
Not until recently, more long-term scientific evidences5 were presented to acknowledge the immediate post-extraction implant placement which is a predictable implant alternative with a survival rate similar to that of the conventional technique for implant placement. And yet it still categorized as a high risk of implant failure in comparison to delayed implants14.
CHALLENGES OF COMPLEX SITES & FRESH EXTRACTION SOCKET FOR IMPLANTATION
In this series, complex sites were categorized as severely resorbed post-extraction sockets or pre-extraction sockets with local infection due to dental pathosis and other ridge deformities, including cleft alveolus, post-tumor resection sites, or failed localized grafted sites. This also includes patients with a history of cancer after chemotherapy or radiation therapy that might complicate the implant surgery outcome. Therefore, a thorough understanding of the biophysiological changes for dental extraction sockets and socket preparation is the cornerstone of success.
Fresh extraction sockets as implant recipient sites pose a great challenge for the primary stability of implant placement in addition to their continuous physiological remodeling. Following tooth extraction, the biological cascade commences with alveolar bone resorption both vertically and horizontally, resulting in gingival collapse, followed by complete bone filling of the socket with signs of radio-opacity similar to the adjacent bone at 105 days. Schropp et al. estimated that two-thirds of the hard and soft tissue changes happen in the first 3 months. In a long-term study, alveolar bone shrinkage could be 40%-60% in height and width within the first 2 to 3 years.
Immediate implants in fresh extraction sites definitely offer alveolar bone maintenance, though the concept of alveolar bone preservation is debatable. A more recent animal histomorphology study demonstrated that implants immediately placed after tooth extraction fail to preserve the alveolar crest of the socket irrespective of their design and configuration. Even so, bone resorption of the buccal crest is more pronounced when placing large-sized implants (5 mm root-formed implants) compared to cylindrical implants with a smaller diameter (3.3 mm). In the same study, the residual defect surrounding the smaller size implant was found to be larger when compared to the larger size implant group once osseointegration was achieved. The necessity of implant-socket gap management is fully illustrated by the evidence of a 50% reduction in the original horizontal bone thickness following facial/buccal bone remodeling. Conversely, those with adjunct bone augmentation exhibited significantly reduced horizontal resorption of buccal bone. Furthermore, Botticelli et al. found that a 1-1.25 mm wide peri-implant gap defect healed uneventfully with or without a membrane. Therefore, we decided to standardize the adjunct treatment for implant-socket gaps >1.5 mm for grafting of the gap to attain better long-term outcomes.
Insertion torque is crucial for implant success and survivability, especially for immediately loaded single implants. Different implant designs can reach various ranges of insertion torque. Akca et al. showed that the insertion torque values for Straumann® and Astra Tech™ implants were as high as 57.6 Ncm and 68.5 Ncm, respectively, in the anterior mandible (type I dense cortical bone), while the values dropped to an average of 10.7 Ncm and 6.4 Ncm in the posterior maxilla (type IV soft bone). An in-vitro experiment showed that BLX implants could be appropriately applied in implant recipient sites that lack cortical bone, such as the posterior maxilla, and could be preferred in cases with type IV bone. Moreover, clinical reports showed that immediate implant placement at the fresh extraction socket (where initial stability is generally compromised) could achieve insertion torque above 50 Ncm.
Insertion torque is crucial for implant success and survivability, especially for immediately loaded single implants. Different implant designs can reach various ranges of insertion torque. Akca et al. showed that the insertion torque values for Straumann® and Astra Tech™ implants were as high as 57.6 Ncm and 68.5 Ncm, respectively, in the anterior mandible (type I dense cortical bone), while the values dropped to an average of 10.7 Ncm and 6.4 Ncm in the posterior maxilla (type IV soft bone). An in-vitro experiment showed that BLX implants could be appropriately applied in implant recipient sites that lack cortical bone, such as the posterior maxilla, and could be preferred in cases with type IV bone. Moreover, clinical reports showed that immediate implant placement at the fresh extraction socket (where initial stability is generally compromised) could achieve insertion torque above 50 Ncm.
When planning for immediate implant placement in a fresh extraction site, several preoperative parameters need sufficient anticipation, such as the reasons for tooth loss, peri-apical health status, and implant size matching. The reason for tooth loss could be a prognostic factor of the implant treatment which truly reflects the patient’s oral functional status. All our patients submitted for immediate implant placement underwent CT digital planning. Implant-socket dimension matching in coronal and apical bony engagement could be well anticipated, especially in the lower molar socket with the inferior alveolar nerve below. Yet, a 4.5 mm or above platform width and at least 12 mm implant length were found to be the most used fixtures in our series for premolar and molar immediate post-extraction fixture installation, accounting for 84.6% (11/13) of cases. (Table 1)
Peri-apical infection is not a contraindication for immediate implant placement. Though the occurrence of peri-apical lesions on implants and implant loss showed a clear linkage to a history of endodontic or peri-apical pathology. Adequate pre-operative antibiotic therapy and meticulous local debridement are essential in addition to adequate insertion torque.
Amongst 19 immediate implants, 8 were temporarily restored and functioned immediately. The decision for either immediate temporization and function or staged procedures was balanced by patient concerns, dental segment location, status of the extraction socket, and primary stability achieved. We adopted a flapless approach for most of our patients except for those implant sites with severe buccal bone loss that needed bone augmentation and were close to vital structures such as the mental foramen. The flapless approach for implantation is technique-demanding and not suitable for cases where gingival contour needs significant labial augmentation. It is always necessary to anticipate labial soft tissue contour stability as the physiological and predictable loss of facial bone might lead to marginal recession of the peri-implant mucosa. With the advent of imaging technology, Cone Beam CT studies showed dimensional changes to the peri-implant facial bone in maxillary anterior single immediate implant placement and temporization at both horizontal and vertical areas.
SPECIAL FEATURES OF BLX IMPLANT FOR IMMEDIACY & COMPLEX SITES IMPLANTATION
SPECIAL FEATURES OF BLX IMPLANT FOR IMMEDIACY & COMPLEX SITES IMPLANTATION
Though various studies33,34 showed platform switched implants could achieve a much stable marginal bone level and highly satisfactory esthetic result. The reduced neck diameter of BLX implant10 is a build in platform switch design to enhance peri-implant osseous gingival support that should be an optimal design for immediate placement at aesthetic - demand region. The design of BLX Implant is a bi-directional bone cutting implant with variable thread. It could perform controlled compaction and densification of the peri-implant bone that could provide idea primary stability in all types of bone10. Moreover, posterior maxilla and type IV bone region or complex sites are lack of cortical bone that BLX implant seems to be prudent choice by extrapolation of this in-vitro experiment24. For complex site in upper molar region, short and wide based BLX found to be an excellent self-drilling implant with round apex with engaging thread help to lift the Schneiderian membrane of maxilla sinus after cut through the socket base meticulously. In an animal study35 showed SLActive® surface is associated with an increased anti-inflammatory macrophage response during early healing phase that contributes prompt bone healing especially in medical compromised subjects. Clinical studies36,37,38 showed superb implant survival rate for SLActive® surface implant in both diabetic patients and oral cancer patients receiving irradiation therapy.

CONCLUSION
This clinical report reviewed 30 months of experience using Straumann® BLX dental implant rehabilitation with good clinical outcomes in a Hong Kong private implant practice. Complex sites and immediate implant placement in fresh extraction sockets demand exceptional dental implant design and high insertion torque to achieve promising primary stability and accelerate osseointegration. The variable bone cutting thread, high insertion torque, SLActive® surface, and versatile implant body width and length options are the salient features. Nowadays, with the biomechanical innovation of implant design, complex sites and fresh extraction socket treatment outcomes have become an essence rather than a challenge to immediate dental implant systems.