ROBOTIC SURGERY AND MEDICINE
Robotic surgery, started to enter scientific application in the mid-eighties of the previous century, through research on telesurgery in war and in space exploration. As space exploration was expanding with potential permanent placements of humans in new frontiers such as the International Space Station and remote commands, there was a great interest for the development of telemedicine services, including tele-surgery. Initial attempts of telesurgery however, were greatly limited by infrastructure problems such as signal transmission and delay and progress was slow for the first decades. The COVID-19 pandemic, catalysed a rise of medical and surgical robotic applications, as innovation was pushed by the urgent need to prevent transmission of the viral disease and reduce exposure of the frontline healthcare providers to the contagious environment.
Today, the surgical robot is an established reality in fields like orthopaedics and neurosurgery and is rapidly becoming a disruptive innovation in several fields of surgery and healthcare.
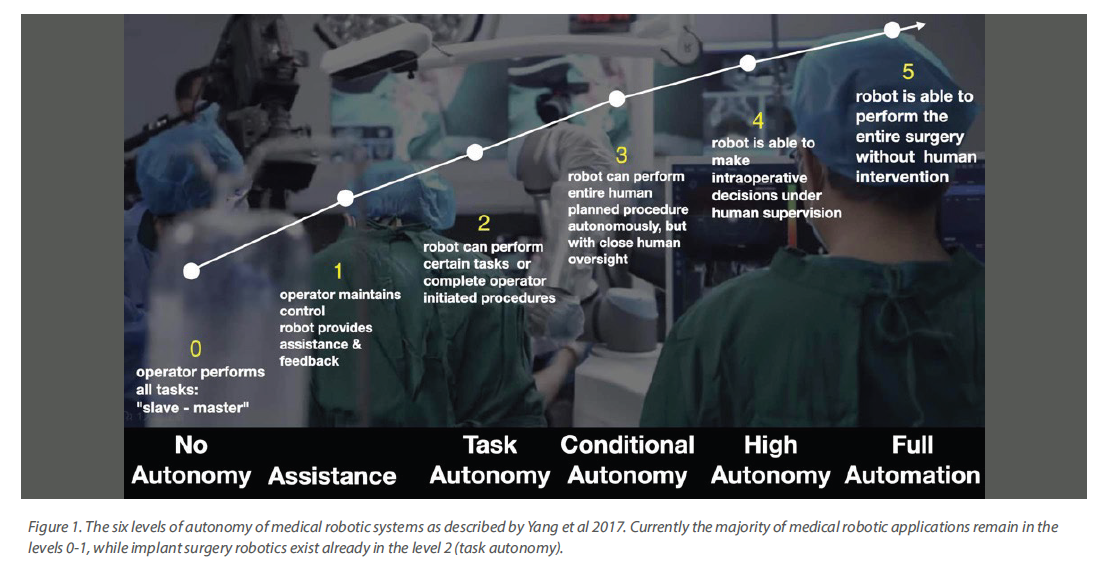
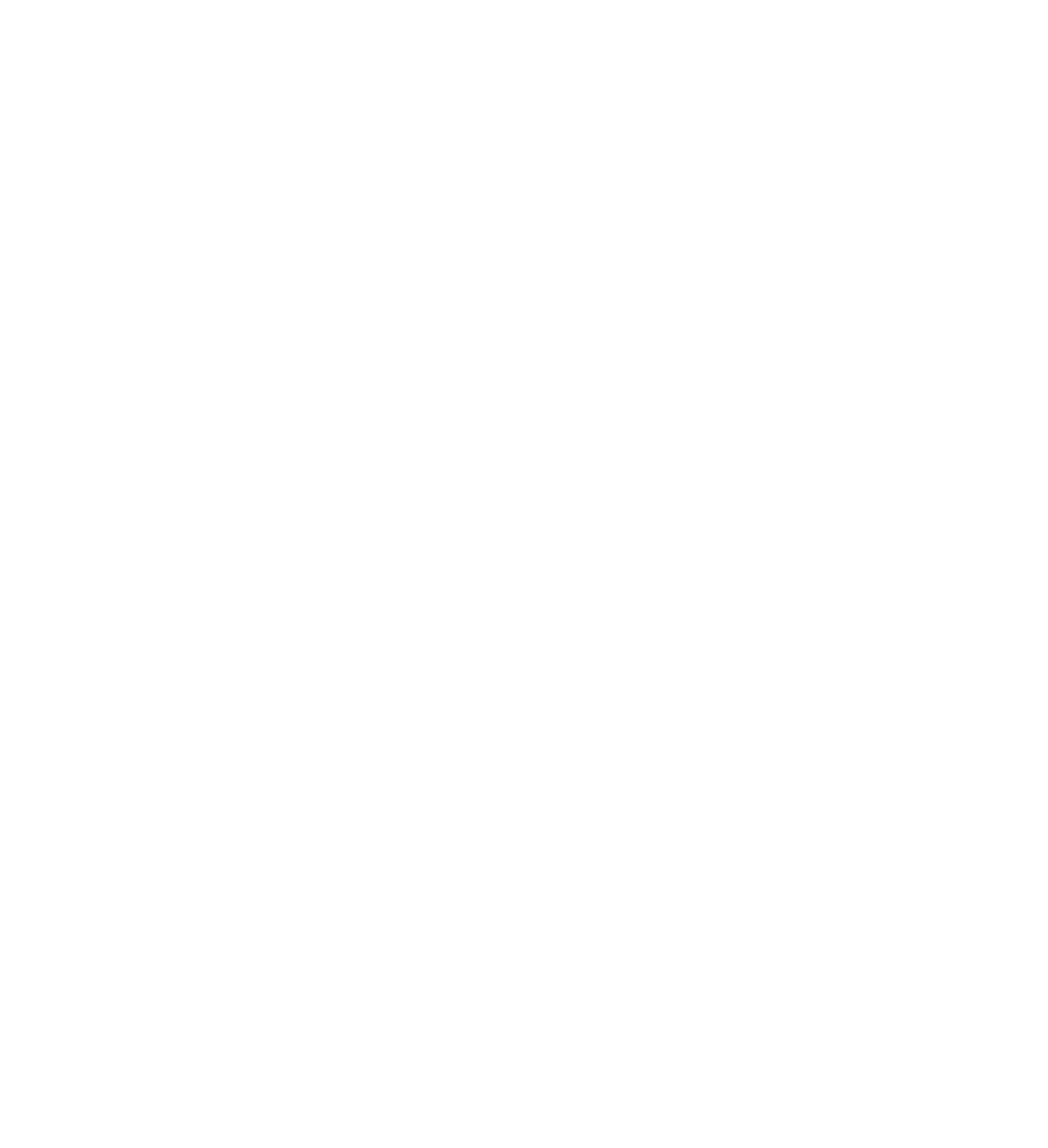
Currently, medical robots can be categorised in six levels based on their autonomy of operation: from the lowest levels of 1)“no autonomy” and 2)“assistance”, intermediate levels of 3)“task”, 4)“conditional” or 5)“high” autonomy to the highest level of 6)“full automation” (Yang et al 2017) (Figure 1). At present the available robotic systems specific for implant surgery are either robot-assisted (level 2: assistance) or autonomous with task autonomy (level 3). The first category, often referred to as remotely operated or “tele-controlled” type of surgical robots, is widely applied in orthopaedic surgery and the surgeon has control of the robotic arms during the whole operation through a console by means of bimanual wrist manipulation. Da Vinchi was the first robotic system which received US Food and Drug Administration (FDA) approval in 2000 for laparoscopic surgery, while the same system was approved in 2009, for transoral procedures in all benign diseases, selected malignant lesions and surgical management of obstructive sleep apnea (Wu et al 2019).
Both remotely operated as well as task autonomous robotic applications currently exist in implant dentistry. The autonomous robotic surgery is an extension of the optical tracking technology of the dynamic CAIS coupled with the robotic arm, while haptic technology is utilised in the operator controlled robotic system. While optical tracking is vision-based, in haptic guidance a robotic arm assists in precise and automatic positioning of the dental handpiece by attaching a separate robotic extension to the patient’s jaw for coordinate measurement.
In the autonomous robotic category however, implant robots employ a robotic arm to carry a handpiece and conduct the osteotomy and dental implant placement under human supervision but with no active guidance. Thus, autonomous robotic CAIS could combine the benefits of the static and the real-time image-based guidance of the dynamic CAIS. The robotic arm is a steady and precise mechanism which can eliminate any human operator related limitations by ergonomics, reduced field of vision, fatigue or tremor and thus increase precision.

WHAT IS THE CURRENT STATE OF ROBOTICS IN IN IMPLANT SURGERY?
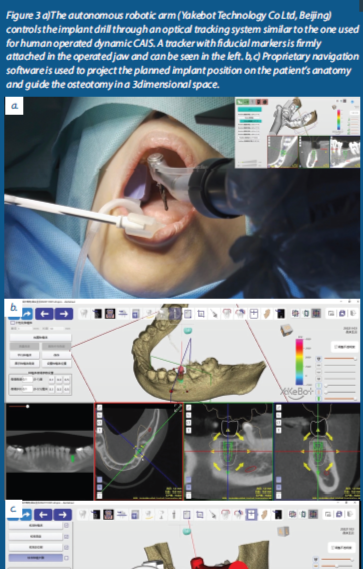
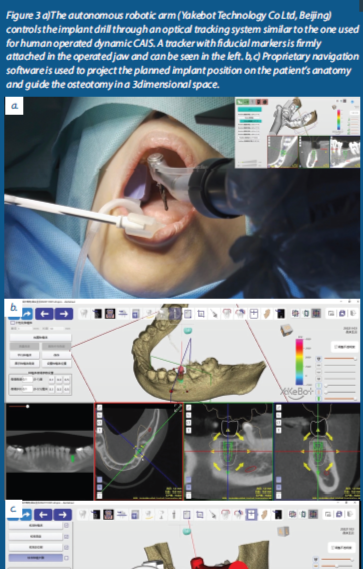
Robotic Implant Surgery is a disruptive innovation even by the standards of medical robotics. Unlike the great majority of robotic applications in medicine which remain mainly in the “slave – master” level of autonomy, dental implant robots have “leapfrogged” straight to task autonomy (Figure 2), being currently in the forefront of development for the entire field. The world’s first autonomous dental implant robotic placement, was successfully conducted in 2017 by Peking University (Beijing, China) and the Fourth Military Medical University Hospital (Xi’an, China). Commercial launch of the robotic system followed in 2021 as Yakebot (Yakebot Technology Co Ltd, Beijing) (Figure 3). According to the manufacturer, the purpose of producing an autonomous robot for dental implant surgery was to minimize any human errors during surgery and to address the shortage of qualified dentists in China. Yakebot system consists of a serial robotic arm, a navigation system, a dental implant handset and the DentalNavi (Yakebot Technology Co Ltd, Beijing) software (Figure 3a-c). A second robot was registered in China for autonomous placement of dental implants in 2019 under the name Remebot (BeiJing BaiHuiWeiKang Co., LTD), which has also by now published clinical documentation (Figure 4). In the United States, a dental implant robotic system called YOMI received FDA-approval in 2017. YOMI is a robotic system using haptically guided stereotactic robotic technology, which can direct the osteotomy based on the planed preoperative trajectory. YOMI delivers physical guidance by constraining the drill position, orientation, and depth, while simultaneously preventing deviation of the surgeon’s hand by means of vibrational feedback. It is based on the physical human-robot interaction to ensure safe movement of the robotic arm during operation; thus, it could be categorised as robot-assisted placement (assistance level).
WHAT IS THE CLINICAL EVIDENCE OF ACCURACY OF ROBOTIC IMPLANT PLACEMENT?Autonomous robotic implant surgery is still at an infancy, albeit certainly beyond the proof-of-concept stage. Apart from numerous
in-vitro and simulation studies, clinical evidence is presently available in the form of case studies (Moser 2020, Yang et al 2022) or series (Chen et al 2023, Yang et al 2023, Bolding and Reebye 2022), including complex edentulous cases of immediate placement and loading.
Yang et al 2023 in a case series with autonomous robotic placement of single implants in 10 patients with the system Remebot, reported a mean overall deviation of 0.74 mm at platform, 0.73 mm apical 1.11◦ in the angle. Similarly, Chen et al 2023 utilised a robotic arm to place 31 implants in 28 partially edentulous patients, documenting a mean angle deviation of 2.81 ± 1.13°, while the 3D deviations at the implant shoulder and apex were 0.53 ± 0.23 mm and 0.53 ± 0.24 mm respectively. Such levels of accuracy would be lower than the current benchmarks with human-operated static and dynamic CAIS (Pellegrino et al 2021) and comparable with the accuracy reported from the few studies combining static and dynamic CAIS in single gaps (Yotpibulwong et al 2023) and edentulous patients (Tahmaseb et al 2018,) respectively. The first case of full arch implant rehabilitation with immediate loading is now reported also with autonomous robotic system. Yang et al 2022 utilised Remebot to place six implants in the edentulous maxilla and to immediately load them with a full arch prosthesis. The process was more complex and required a personalized mucosa-supported template with an optical positioning marker and a tooth-supported guided template, which were fixed together with metallic pins. The template with the positioning marker was secured to the patient jaw using bone screws. The implants were placed in the maxilla with mean coronal and apical deviations of 0.59
+/- 0.24 mm and 0.61 +/- 0.23 mm respectively, while the mean angular deviation was 0.89 +/- 0.38 degrees.
Bolding and Reebye 2022, assessed the accuracy of implant placement in five patients with the YOMi haptic robotic system. They assessed a total of 38 implants placed in 8 edentulous dental arches, showing an average global angular deviation of 2.56 +/- 1.48 degrees, and deviation at the entry and apex of 1.04 +/- 0.70 mm and 0.95 +/- 0.73 mm respectively. Such accuracy would be at least as good as results achieved with human operated static or dynamic CAIS in similar cases.
FUTURE DIRECTIONS
About five years after the first autonomous robotic dental implant placement and this technology has achieved remarkable progress with two types of robotic systems already commercially available in US and China. Although the clinical application is currently limited, the emerging evidence suggests the technology is already beyond the “proof of concept”. Many witnessed the first robotic implant placement through the news as a “publicity stunt” with little if at all impact in the way we will be practicing implant dentistry. Yet the fast pace of progress of this technology has taken many by surprise. Case series have demonstrated accuracy of placement which appears higher than this achieved by human operators, even when CAIS is utilised and in complex cases such as the edentulous arch. Nevertheless, the high costs and complexity of this technology, as well as the need for human intervention (task autonomy only) and direct supervision currently limit its application into mainstream practice. However, upcoming developments and improvements in the technology might soon change this.
The robotic arm remains a flexible and precise operator. Adding functionality and procedures to the robotic arm is just a matter of installing a software update. In the future, expanding the use of robotic arms to other surgical and non-surgical procedures could increase the indications and thus the benefits of such a system for the whole clinic. A robotic arm could easily be programmed to use an optical scanner for example, acquiring patient intraoral scans in an unmanned scanning station. A robotic device for crown preparations of natural teeth is already developed and validated
in-vitro (Yuan et al 2016), a development which could be the next frontier within reach of clinical application. Coupled with advances in machine learning and artificial intelligence, new possibilities could emerge for autonomous robotic surgical applications, allowing wider implementation in implant dentistry.
For now, an experienced implant surgeon remains irreplaceable; and this will not change in the foreseeable future. However, a future where robotic machines will have an ever-increasing role in surgical procedures is already visible!